DIGESTIVE SURGERY
The clinical outcomes (short-term and long-term) of patients with diseases in certain anatomic areas of the body have dramatically improved since the time that these areas have been dealt with by surgeons with a proven, dedicated, and long-standing interest, training and experience in these particular areas (i.e.: breast surgery, endocrine surgery, etc). During the last decade in the USA, the UK, and elsewhere there has been an increasing number of divisions of surgery dedicated to the digestive system alone. This trend is based on the proven fact that even a “simple” and common abdominal operation (such as a right hemicolectomy for example) is performed more “radically” (wider healthy margins, significantly more lymph nodes resected), safer (fewer complications, faster recuperation), with better prognosis (5-year survival, disease-free survival, cure), and cheaper (shorter hospital stay, quicker return to work) by a specialized gastrointestinal surgeon compared to the usual “general” surgeon. The above mentioned scientifically proven and widely recognized facts become a lot more pronounced when one considers much more challenging diseases and anatomic areas, such as the esophagus, stomach, pancreas, liver, and rectum, which had been traditionally dealt with by “general surgeons” in a totally empiric way (depending on each one’s individual experience, based on “try-and-error” methods). Contrary to this old pattern of practice, the gastrointestinal surgeon with qualifications, credentials, and proven long dedication to this field, has acquired specialized experience with a large number of operations on the esophagus, pancreas, liver, etc, but also practices evidence-based surgery, which means that the indications for surgery, its timing, preoperative treatments, operative technique and technology, postoperative care and treatments are all driven by guidelines and algorithms developed by international teams of the true experts.
WHERE TRUE DIFFERENCE IS MADE
These are some of the areas where a specialized gastrointestinal surgeon does make a difference:
1. Lymph node dissection. The accurate staging, outcome and prognosis of patients with abdominal tumors (of the stomach, pancreas, colon) depend not only on the appropriate resection of the affected part of an organ, but also largely on the extent of lymph node dissection, that is on the number of lymph nodes resected around the tumor and the organ. The oncologic significance of the lymph node ratio is widely recognized today, and this becomes stronger as the number of lymph nodes resected becomes higher.
2. Resection of the portal vein and/or the superior mesenteric vein that may be infiltrated by cancer of the pancreas and replacement with a graft. Generally, tumors of the pancreas involving these vessels are considered “unresectable”, or “inoperable”, except if the surgical team has the experience and the expertise to excise the tumor along with the involved part of the vein. This is what makes the critical difference between getting rid of a pancreatic tumor or not.
3. Total mesorectal excision (TME). In patients with cancer of the rectum it is essential to take out not only the tumor-bearing part of the rectum, but also the whole fatty tissue all around it. Patients with TME have dramatically better long-term results compared to those who have only the tumor taken out.
4. Transhiatal Esophagectomy. When the whole esophagus needs to be removed in cases of cancer, it makes a big difference to be able to perform this operation without making an incision in the chest. This leads to shorter hospital stay, far less complications, and much earlier recuperation.
5. Tailoring of Fundiplication in patients with gastroesophageal reflux disease. Such patients may need different types of operations depending on the precise function of each one’s individual esophagus.
6. Less trauma during an operation. When challenging operations are performed by surgeons who have performed a large number of them, then the technique is very standardized, a lot fewer blood transfusions are required, significantly fewer complications occur, need of ICU is more rare and shorter, and hospital stay is cut shorter as well.
7. Long-term outcome. When evidence-based surgery is practiced, certain treatment algorithms are followed, the operative technique is standardized and incorporates a large surgical experience, then the long-term outcome and quality of life are dramatically improved.
A SPECIALTY ON ITS OWN
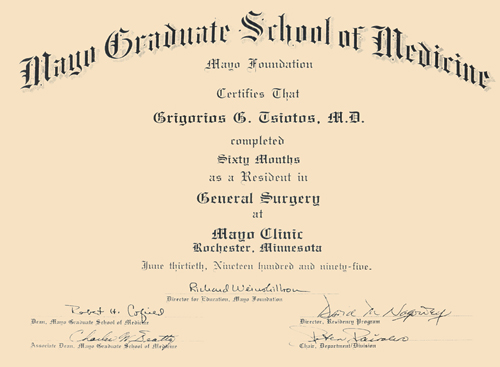
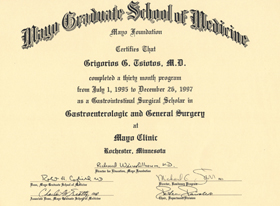
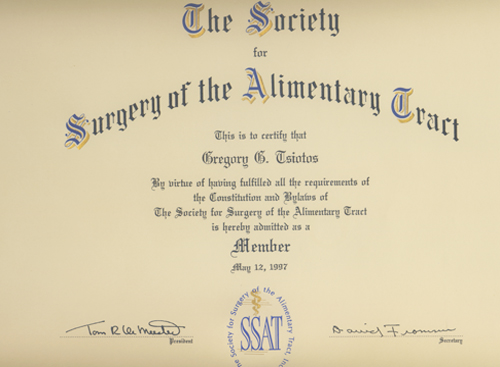
Digestive surgery or gastrointestinal surgery was recognized as an independent subspecialty in the USA during the mid-90’s. At that time there were four (4) institutions that offered this subspecialty, as a fellowship after five years of General Surgery training. These were the Mayo Clinic, the Cleveland Clinic, The Johns Hopkins, and The Virginia Mason Clinic. Since 2000, these institutions gradually increased and now they are up to twenty. In the USA and in the rest of the world, such a certification is considered a very strong and sought-after credential. Several hospitals around the world have been making every effort to establish a Department dedicated to Digestive Surgery, because it is well understood that by doing this, they can advance to the level of a “referral center of excellence” for very challenging diseases and operations. Digestive surgery is walking its own way academically as well. The Society for Surgery of the Alimentary Tract (SSAT), although created 30 years ago by some surgical pioneers and visionaries, it has recently become the most prestigious and highly respected forum for discussions on the science and art of surgery of the gastrointestinal system universally. Accordingly, its official journal, the Journal of Gastrointestinal Surgery is now the most highly respected scientific publication in this field.









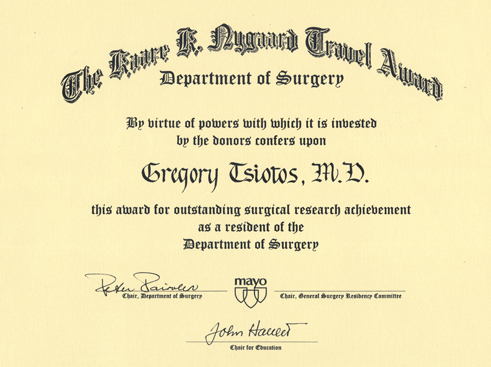
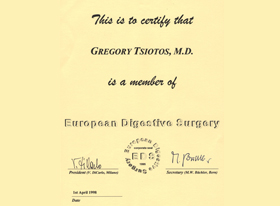
 Since the beginning of my surgical training at the Mayo Clinic (1990-1995), I developed a very strong interest for the surgery of the pancreas, liver, and all gastrointestinal system. In 1995, I was one of the only four (4) young surgeons in all USA to be accepted for a highly specialized fellowship in gastrointestinal surgery. This took place also at the Mayo Clinic (July 1995-December 1997). Subsequently, I accepted the position of Assistant Professor of Surgery at the University of Missouri (March 1998-February 2000) and the Director of the Division of Upper Gastrointestinal Surgery, just created there. During these two years, the number of patients operated on there for pancreatic, liver, esophageal and gastric diseases was increased fivefold. This not only reflected the highly specialized and advanced experience gained at the Mayo Clinic, but also the strong potential that a specialized division dedicated on gastrointestinal surgery carries with it. Up to the present time, there is no other such department of surgery in Greece and southeast Europe, devoted to the exclusive practice of digestive surgery at the highest possible level. One of the reasons is that there are extremely few surgeons in the world with such a specialized qualification, received at, what many people consider as, the best medical referral center in the world.
Since the beginning of my surgical training at the Mayo Clinic (1990-1995), I developed a very strong interest for the surgery of the pancreas, liver, and all gastrointestinal system. In 1995, I was one of the only four (4) young surgeons in all USA to be accepted for a highly specialized fellowship in gastrointestinal surgery. This took place also at the Mayo Clinic (July 1995-December 1997). Subsequently, I accepted the position of Assistant Professor of Surgery at the University of Missouri (March 1998-February 2000) and the Director of the Division of Upper Gastrointestinal Surgery, just created there. During these two years, the number of patients operated on there for pancreatic, liver, esophageal and gastric diseases was increased fivefold. This not only reflected the highly specialized and advanced experience gained at the Mayo Clinic, but also the strong potential that a specialized division dedicated on gastrointestinal surgery carries with it. Up to the present time, there is no other such department of surgery in Greece and southeast Europe, devoted to the exclusive practice of digestive surgery at the highest possible level. One of the reasons is that there are extremely few surgeons in the world with such a specialized qualification, received at, what many people consider as, the best medical referral center in the world.