Gastroesophageal Reflux Disease – Hiatal Hernia - Esophagitis
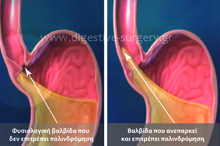
Gastroesophageal Reflux Disease, or GERD, is very prevalent in the western world, as it affects, in various degrees, about 20% of the population. Its cause is the malfunction of the so called “lower esophageal sphincter, or LES, which allows the stomach contents to reflux back into the esophagus. Since the stomach contents are normally very acidic, their abnormal presence in the esophagus causes inflammation, called esophagitis. In addition, it causes symptoms, such as chest pain, heartburn, or bitter taste. Patients who have more advanced disease may experience actual food reflux into their mouths, especially when they are in bed. There are certain substances that are known to further abnormally relax the LES and thus they are associated with worsening of the symptoms. These are: fat, alcohol, caffeine, chocolate, and nicotine.
Hiatal Hernia and GERD
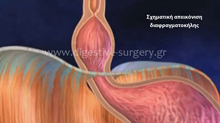
As the esophagus comes down through the chest into the abdomen, it has to go through a relatively flat muscle, called the diaphragm. Normally there is an opening in the diaphragm, big enough to comfortably accommodate the size of the esophagus. In some people, this opening becomes abnormally wider. Because of the intra-abdominal pressure, which is higher than that of the chest’s, part of the stomach may be “pushed upwards” through this opening, into the chest cavity. This is called: hiatal hernia. The presence of hiatal hernia is always associated with GERD, but the opposite is not necessarily true, since not all patients with GERD have a hiatal hernia at the same time.
Symptoms
Most commonly, patients complain of chest pain, bitter taste in their mouths, and a “burning” sensation in their stomach or the chest (“heartburn”). Such symptoms may become even worse after a meal, especially a heavier one. As the disease becomes worse with time, patients may experience regurgitation of food back up to their mouth. This is not the same as vomiting, since it is not associated with nausea and with this forceful evacuation of stomach contents through the mouth. Patients usually describe this condition as food simply “coming up backwards”. In some very advanced cases, patients may suddenly wake up panicked at night, with a feeling of “suffocation” because the food, which refluxed back up through the esophagus, has gone down again, but this time into the trachea (the “breathing pipe”) and then in the lungs. All these speak to the fact that GERD is not always this “innocent heartburn that goes away with a pill”. The continuous irritation of the esophagus, caused by the chronic reflux of the acidic stomach contents, results to severe inflammation of the esophagus (esophagitis), which, if left unrecognized and not appropriately treated, may lead to a precancerous state, called “Barrett’s Esophagus”. Again, if this latter condition is not definitively treated, it may progress to cancer of the esophagus, a disease with bad prognosis.
Asthma and GERD
It is very interesting (and well recognized today) that many patients who suffer from “asthma” for years actually have GERD. We now know that the frequent reflux of really very small quantities of acidic stomach contents (not more than drops), up into the esophagus and down the trachea and the lungs causes continuous irritation of the smaller branches of the trachea (called “the bronchi”), and thus “bronchial asthma”. Patients with bronchial asthma in whom no allergic or other cause has been proven, should be tested for GERD. Similarly, people who complain of otherwise unexplained hoarseness of breath, or bad teeth, should also be tested for GERD.
Management
Most patients benefit from medical management. This generally consists of the appropriate medication, in addition to some diet and lifestyle changes. The medication neutralizes the acid of the stomach, which of course keeps on refluxing into the esophagus, but it is not as irritating as before. Because of this, patients feel that their symptoms improve. It is important to emphasize that the medication does not the disease of reflux, but only its symptoms. In addition, patients should avoid certain diet contents (fat, alcohol, caffeine, chocolate) and make some lifestyle changes (quit smoking, not going to bed before 3-4 hours after their last meal of the day), etc. The definitive treatment of patients in whom GERD persists despite appropriate medical therapy is the laparoscopic repair of the hiatal hernia and the fundoplication of the stomach, which takes care of the actual cause of this disease; not just the symptoms.